Immunoassays are biochemical tests that are used to quantify the presence and amount of specific macromolecules or analyte in body fluid. These tests are specific and quite sensitive because of the purified antibodies or antigens used as reagents.
Immunoassays are mainly used in measuring drugs, hormones, tumor indicators, cardiac injury indicators, specific proteins and drugs. Qualitative immunoassays are used to detect the presence of antigens of infectious diseases and antibodies produced to combat them.
For example, if an antibodies of Lyme disease or HIV are detected in a person, they are indicators that that person has the disease. The body fluids that will commonly be used for this test are blood, urine, and cerebrospinal fluid.
These tests are also vital in the detection of the antigens of Streptococcus and Cryptococcus, using the cerebrospinal fluid in patients with meningitis, and of Hepatitis B.
Procedure
In order to carry out an immunoassay test, the specific antigen is included in the testing system. If the antibody the test is designed for is in the fluid sample, it will link to the antigen that is present in the test. This means that the result is positive. On the contrary, if there is no reaction or linking, it means that the result is negative.
Examples of assays for specific antibodies include the rheumatoid factors. They are used as a marker in individuals with suspected rheumatoid arthritis (RA) or other autoimmune conditions. It can also be used to ascertain the efficiency of the vaccination against Hepatitis B.
Whenever an immunoassay test is used to check for antigens in body fluid, like blood or cerebrospinal fluid, the test has antibodies that can actively link with the antigen in question. The antigen’s reaction when present in the patient’s sample to a particular antibody is placed side by side with the reactions of other verified concentration and then the quantity of antigen is reported.
Some of the assays for detecting antigens are drug levels (example include vancomycin and digoxin), hormone levels (such as TSH, estrogen, and insulin), and cancer indicators like AFP and CA-125.
Here are the usual steps to run an immunoassay test:
- Choose the best type of technique for the test: To determine what technique you would use, you have to put into consideration the cost, requirements, and sensitivity of the test. Also, determine the environment you want to carry out the test in.
- Choose the antigen-antibody pair for testing: You need to check for the availability of the materials for your test and get them in the market or generate them yourself in the lab.
- Bind your antibody or antigen to a sterile surface: The surface can be a lab bead or plate depending on what you are doing exactly and depending on your technique (sandwich antibody probing or competition assay).
- Optimize your washing steps and blinding so that non-specific bonding would be minimized.
- Incubate your antibody or antigen with a secondary molecule.
- Use a trusted guideline to validate the efficacy of your procedure.
Types of Immunoassays
There are five types of immunoassays:
- Counting Immunoassay: In this assay, polystyrene beads are covered with antibodies that should link with the expected antigen. As the beads are incubated, they link to antigens and clump together. Some however do not link. The whole solution is passed through a counter and it takes note of the number of unbound beads. The number of unlinked beads is inversely proportional to the antigen amount.
- Radioimmunoassay: This is the first-ever type and it makes use of a radioscope that is linked to the expected antigen and covered with a complementing antibody. The body fluid sample is added and it competes with the antigen and replaces it. The unbound antigens are washed away and radioactivity of the fluid is measured. The target antigen amount is inversely proportional to the level of radioactive signal.
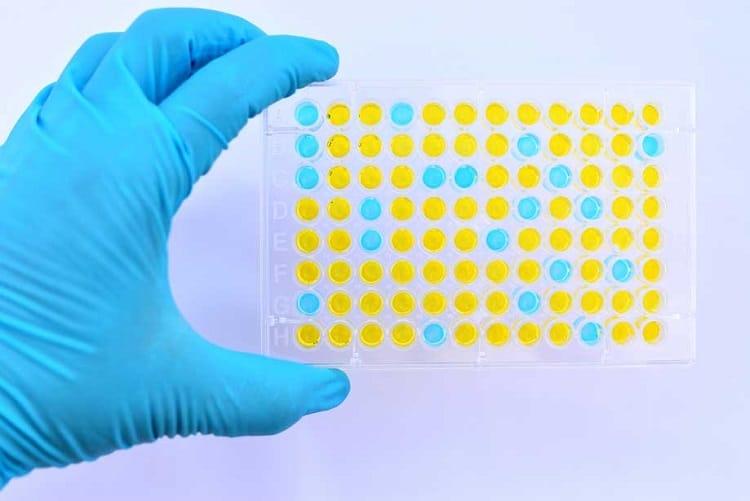
- Enzyme-linked immunosorbent assay: Unlinked antibody is washed off after incubation with antigen and the linked antibody-enzyme attached to the antigen is joined with a substrate. The enzymes then facilitate a chemical response and their color changes. This is what is used to check for CD4+ cells when diagnosing for AIDS.
- Chemiluminescence immunoassay: This is just like the ELISA only in which light is released instead of color. This test was originally invented to diagnose zika virus.
- Flouroimmunoassay: The antibody is stuffed with fluorescent probes. After incubation, the antigen-antibody mix is separated and the intensity of the fluorescents are measured.
Researchers are steadily looking for ways to improve on immunoassays but for now, these are the methods currently being used.
Blood Removal and Storage
The blood sample for the test is collected by puncturing the vein using a needle and the blood is stored in tubes without additives. Do note that not all of the blood is used for the test. The blood is left to rest at room temperature for 30 minutes and then spun with a centrifuge at 2000 rotations per minute for ten minutes. The resultant serum, called the supernatant because it stays on top, is collected ad stored at -80 degrees Celsius.
Conclusion
Immunoassays are highly sensitive tests that are important to detect many deadly illnesses. These tests are run by highly qualified personnel under strict test conditions. However, there are sometimes cases of false positives that occur mainly as a result of human error, so if your doctor doubts the results you may have to take another test.

